TogetherFightingCOVID

TogetherFightingCOVID


Recovery is not a total abstinence but involves a daunting set of tasks. It is an ongoing process that requires changing many aspects of life – how you think, react to certain situations, and cope with emotions created by these aspects of life. A personal recovery plan is one of the first things you need to do after treatment. It involves a set of guidelines, goals, methods, notes, and processes that you set to sustain in recovery without relapse. It is important to be honest with yourself so that you can adapt and continue to create a lifestyle that is conducive to your health and recovery.
Although recovery plans are unique to each individual, there are specific components that are helpful to include in it.
Personal Goals.
You will need to deeply assess your current status and decide upon your major needs and goals. Identify the motivations for making this change, what challenges will potentially be your biggest barriers, and whether you can commit to following those guides in order to change your life. If you can identify your motivations, understand your challenges and recognize that the outcome will be worth the effort, you will be ready to create your plan.
Triggers
A trigger is a person, place, conversation, or circumstance that can cause you to feel the urge to use drug and/or alcohol again. It is necessary to be aware of your triggers, the situations that might bring them about the most frequently, and the best ways to handle them. Some of the triggers are seeing someone that would remind you of drug use, driving by a bar you used to go to, remembering anniversary dates of losses or trauma, losing a job, frightening news events, too much to do – feeling overwhelmed, family friction, the end of a relationship, financial problems, getting a big bill, etc.
Triggers Action Plan
Then develop a plan of what you can do, if a trigger come up, to comfort yourself and keep your reactions from becoming more serious symptoms. Include ways that you can either avoid these situations or alleviate them so as to give you space to cope and overcome them. These may include, taking a different route to avoid the bar you used to go to, staying away from peers, places, and events that center around substance use, play the piano or work on a fun activity, exercise -stretching, playing your favorite sport, or going to the gym, creative activities – painting, sewing, or drawing, etc.
Implement The Plan
It is of great importance to keep to the individual plan daily to support its implementation and manage recovery. Developing a personal substance abuse recovery plan is a great way for an individual to prepare for unexpected challenges during recovery and reply to them in an organized and self-sufficient manner. It can be daunting to devise a way to do these things on a regular basis, especially when you are trying to contend with a life that has changed so drastically. With a recovery plan, a person can establish goals and enact processes that can counter triggers, making it easier to stick to goals and maintain recovery.
Get your life back from substance use. Contact us.
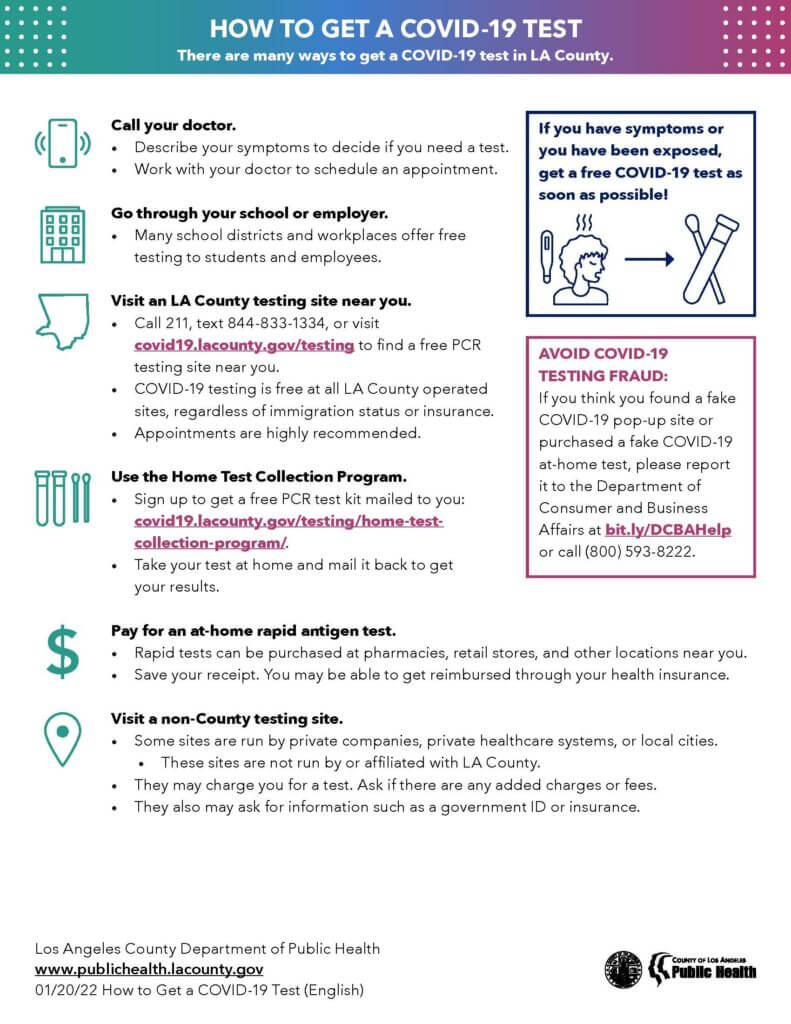
According to CDC, the first confirmed U.S. case of Omicron was identified on December 1, 2021, and as of December 20, 2021, it was detected in most states and territories. Information about Omicron are still new and constantly emerging. CDC expects that anyone with Omicron infection can spread the virus to others, even if they are vaccinated or don’t have symptoms.
We have the Tools to Fight Omicron – CDC
Vaccines remain the best public health measure to protect people from COVID-19, slow transmission, and reduce the likelihood of new variants emerging.
Tests can tell you if you are currently infected with COVID-19.
Masks offer protection against all variants. CDC provides guides on how to select, properly wear, clean, and store masks: –
Check back here for current information from CDC to fight and end this pandemic. Please do your part.
People with substance use disorder are at risk of COVID-19 and its complications. Chronic substance use can harm or weaken the body, including the immune system, in ways that make it more vulnerable to COVID-19 infections. Opioids use act in the brainstem to slow breathing, lung damage caused by smoking is well known, and alcohol use can increase the risk of acute respiratory distress syndrome and pneumonia. These drugs have effects on respiratory and pulmonary health of the individual.
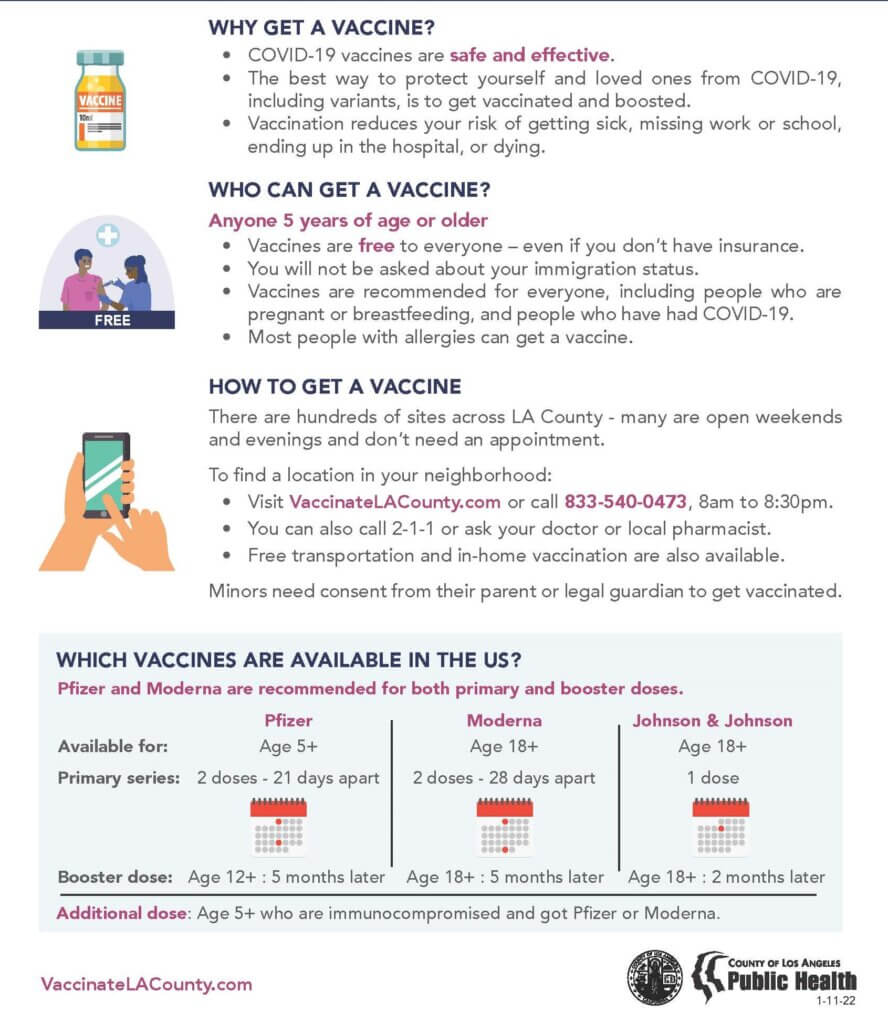
For several months of COVID-19 pandemic people have adjusted to public health and safety protocols as provided by CDC and other public health services departments. The emergence of vaccines, approved by FDA, provided a safety net to the world in saving lives and it seemed as if we have had a control on the pandemic. COVID-19 vaccines have been free and broadly available to adults in US since mid-April 2021. Social and economic activities were returning to normalcy lately until different variants, especially Delta, emerged and created astronomical spikes in cases, hospitalization and deaths. According to the CDC, Delta is about twice as infectious as the original strain and estimated to be 60% more infectious than Alpha variant. Unvaccinated individuals suffer the most.
As we approach the winter months previous health and safety protocols, like mask mandates, are coming back. Social distancing guidance and stay-at-home orders may be returning and that could lead to higher numbers of people using drugs and become vulnerable to COVID-19.
If you or someone you know is in need of support right now reach out to us. We are here to help! We work hard to address access to treatment concerns from our patients and currently implementing a hybrid treatment process – in-person and telehealth!
Cognitive-behavioral therapy (CBT) is a therapeutic approach that seeks to modify negative or self-defeating thoughts and behavior. CBT is aimed at both thought and behavior change (i.e., coping by thinking differently and coping by acting differently). CBT includes a focus on overt, observable behaviors – such as the act of abusing a drug – and identifies steps to avoid situations that lead to drug abuse. When a drug addicted person understands why he feels or acts a certain way, and how those feelings and actions lead to substance use, he is well equipped to overcome his addiction. CBT is about the patient learning to run his life.
In our individual and group treatments, we utilize specialized CBT treatment methods that are tailored for the particular disorder. Our staff acts as a catalyst towards a change by the patient. He creates sessions that feels safe, compassionate and personal and makes the patient understand that the real power rests in his hands.
Once the treatment plan is created, progress can be made with a number of strategies, such as; goal setting, agenda setting, relaxation, problem-solving, behavioral activation, homework assignments, and relapse prevention.
Our comprehensive CBT treatment service is based on the principles that CBT:-
If you or someone you care about is struggling with an addiction to drugs or alcohol, help is available. It’s never too late to make a positive change. Call on us!
The COVID-19 pandemic has turned the spotlight on a tool that has been in use since early days and predominantly used in rural and underserved communities. Although, traditional health service relies on in-person care, the need and want for remote care has existed from the Roman and pre-Hippocratic periods in antiquity. The elderly and infirm who could not visit temples for health care sent representatives to convey information on symptoms and bring home a diagnosis as well as treatment. One of the earliest telehealth encounter can be traced to Alexander Graham Bell in 1876, when he used his early telephone as a means of getting help from his assistant Mr. Watson after he spilt acid on his pants.
The advent of high-speed Internet and the increasing adoption of Information and Communication Technologies (ICT) in traditional methods of care spurred advances in telehealth delivery. Increased access to portable devices, like laptops and mobile phones, made telehealth more plausible.
The Department of Health Care Services (DHCS) defines telehealth as “The mode of delivering health care services and public health via information and communication technologies to facilitate the diagnosis, consultation, treatment, education, care management, and self-management of a patient’s health care while the patient is at the originating site and the health care provider is at a distant site.”
The Federal Health Resources and Services Administration (HRSA) defines telehealth as “The use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration.”
Telehealth utilizes telecommunications and virtual technology. In Divine Healthcare Services, Inc. (DHCS), both the patient and our staff are on HIPAA-compliant video conferencing, so individual patients, groups, and the counselors all see each other.
The Department of Health Care Services and other health care regulatory bodies recommend telehealth services amid this COVID-19 tenuous circumstance. The list of benefits includes, but not limited to:
We utilize guidelines from CDC and Los Angeles County Department of Public Health to implement new procedures to help minimize the risk of exposure to our patients and staff. If you or someone you know is in need of support right now, the DHCS team is here to help.
Understanding Anxiety Disorder
Anxiety is the body’s natural response to stress. It’s a feeling of fear or apprehension about what is to come and it is an expected part of life. When an individual experiences anxiety that is persistent, seemingly uncontrollable, overwhelming, and these anxious feelings begin to interfere with everyday life, it becomes a disorder. Anxiety disorders have one thing in common – the anxiety occurs too often, it’s too strong, and it’s out of proportion to the present situation.
Anxiety disorders are the most common and pervasive mental disorders in the United State, affecting 40 million adults in the age 18 and older, or 18.1% of the population every year. An estimated 31.1% of U.S. adults experience any form of anxiety disorder at some time in their lives
The exact causes of anxiety disorders are not fully understood. Life experiences such as traumatic events appear to trigger anxiety disorders in people who are already prone to anxiety. Inherited traits also can be a factor.
Types
There are several types of anxiety disorders:
Use of certain medications or illegal drugs, or withdrawal from certain drugs, can trigger some symptoms of anxiety disorder.
Someone having an intense fear of being in a place where it seems hard to escape or get help if an emergency occurs. One may panic or feel anxious when on an airplane, public transportation, be in open or enclosed spaces, or standing in or being in a crowd.
A person with GAD feels excessive, unrealistic worry and tension with little or no reason. They may frequently imagine the worst that could possibly happen about future, health, finances, family members, etc.
Separation anxiety is often thought of as something that only children deal with; however, adults can also be diagnosed with separation anxiety disorder. Someone feels scared or anxious when a loved one leaves. Anyone can get separation anxiety disorder. If you do, you’ll feel very anxious or fearful when a person you’re close with leaves your sight and will always worry that something bad may happen to the person.
This is a type of social anxiety in which young kids who talk normally with their family don’t speak in public, like at school. It is often associated with extreme shyness, fear of social embarrassment, compulsive traits, withdrawal, clinging behavior, and temper tantrums.
Someone feels intense fear of specific situations or things that are not actually dangerous, such as heights or flying in an airplane, receiving injections, fear of blood, fear of specific animals. The fear goes beyond what is appropriate and may cause one to avoid ordinary situations.
This is when a person feels overwhelmingly worry and self-consciousness about everyday social situations. A person getting obsessively worries about others judging you or being embarrassed or ridiculed.
When a person feels sudden, intense fear that brings on a panic attack. During a panic attack, a person has sudden and intense physical symptoms like a heart attack. Symptoms can include shortness of breath, heartbeat, dizziness, numbness, or a tingling sensation caused by over-activity in the body’s normal fear response.
Symptoms of Anxiety
The most common symptoms of anxiety include:
Anxiety disorders are treatable, and the vast majority of people with an anxiety disorder can be helped with professional care. One of the measures of treating anxiety disorder is by psychotherapy or “talk therapy”. Cognitive Behavioral Therapy (CBT) is an example of one type of psychotherapy that can help people with anxiety disorders. It teaches people different ways of thinking, behaving, and reacting to anxiety-producing and fearful objects and situations. CBT can also help people learn and practice social skills, which is vital for treating social anxiety disorder.
It can be challenging and frustrating to live with an anxiety disorder and may not go away on their own. They may get worse over time if you don’t seek help. The constant worry and fear can make you feel tired and scared. It’s easier to treat if you get help early. We in Divine Healthcare Services, Inc. are here to help!
Alcohol addiction is a complicated illness that affects each person differently. It can result in many medical complications and can also occur with other mental health and substance abuse disorders creating an increased risk for suicide. People with alcohol addiction drink regularly and in large amounts and when it becomes severe are given the medical diagnosis of “alcohol use disorder” or AUD. They develop a physical dependency over time. When their bodies don’t have alcohol, they experience withdrawal symptoms. There’s no clear cure for alcohol addiction. Overcoming alcohol addiction can be a long process that requires both personal dedication and various treatments or therapies. The optimal treatment plan will depend on personal circumstances, including:
Seeking professional treatment for alcohol addiction is very necessary as quitting alcohol without any type of medical intervention can lead to severe withdrawal seizures and even death. The goal of treatment is to replace negative coping skills and patterns with positive cognitive behavioral skills and coping skills that work for the person. Like any substance abuse or mental health disorder, determining the treatment levels of care is necessary in order to provide the best care. Levels of care range from residential treatment and partial hospitalization to intensive outpatient treatment and regular outpatient treatment.
Here at Divine Healthcare Services, Inc., we understand that what works for one person may not be successful for someone else. We also understand that the rehabilitation process may be longer for some clients than others. That is why we offer a variety of treatment options, ranging from individual counseling and therapy to group support sessions. If you’re ready to face your addiction, make an appointment with us!